When should I consider surgery?
Conservative therapies are less invasive treatments that may offer temporary or permanent pain relief for patients and include
- Activity modification
- Custom orthotics
- Anti-inflammatory medications
- Ultrasound-guided corticosteroid injections (PRP/Amnio Flowable)
If these measures have failed with multiple attempts or when the injury is severe, you may be a candidate for surgical repair.
Surgical Goals and Treatment
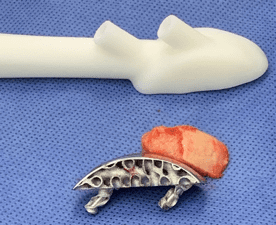
After thorough physical examination and review of your advanced imaging studies, Dr. Cottom and Dr. McAlister will formulate a surgical plan that is tailored to the severity of your injury. The goals for surgical repair are to restore function, reduce pain, and ultimately curb any further progression of ankle arthritis that commonly occur with these injuries.
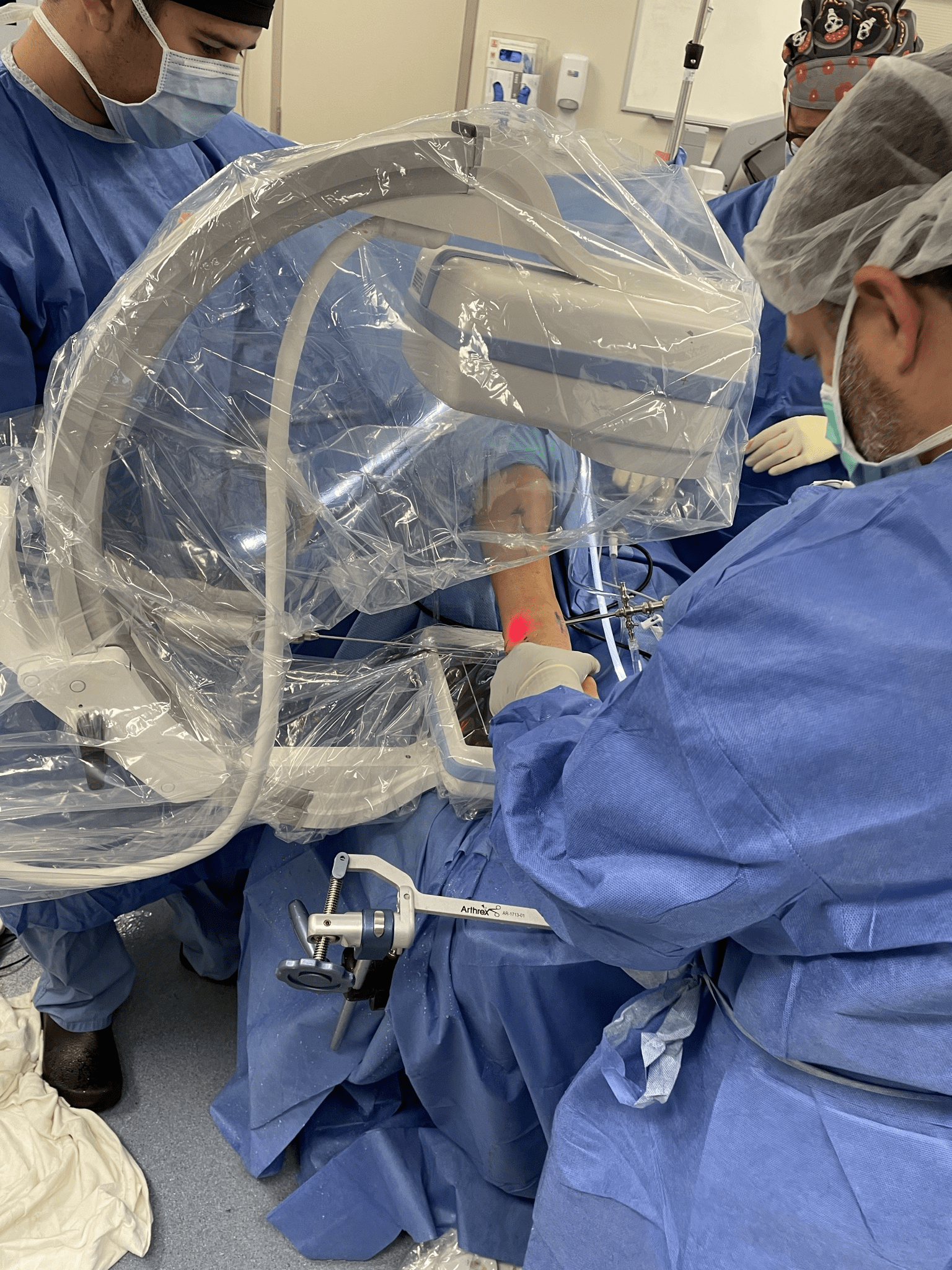
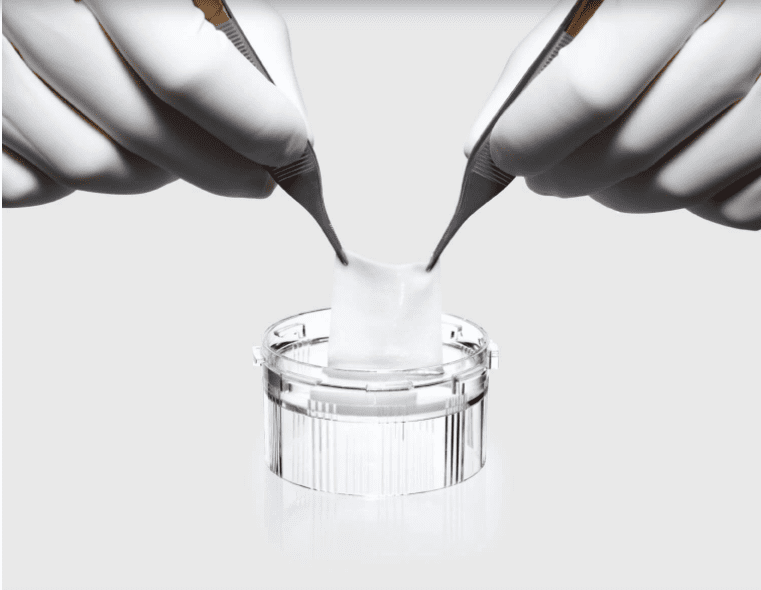
Our team uses minimally invasive arthroscopic techniques to surgically repair osteochondral defects. We first create small incisions to the ankle and inserts an arthroscope, which is a viewing instrument made up of a tiny lens, light source, and camera to enable the surgeon to visually examine the ankle. Arthroscopy allows direct visualization of the ankle joint and avoids any trauma to surrounding structures that would be at risk in a traditional, open approach.